MessageToEagle.com – The development of antibiotics and other antimicrobial therapies is arguably the greatest achievement of modern medicine. However, overuse and misuse of antimicrobial therapy predictably leads to resistance in microorganisms.
Antibiotic-resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistantEnterococcus species (VRE) and carbapenem-resistant Enterobacteriaceae(CRE) have emerged. Certain CRE species are resistant to multiple antibiotics, and have been deemed “superbugs” in the news.

Alternative therapies have been used to treat infections since antiquity, but none are as reliably safe and effective as modern antimicrobial therapy.
Unfortunately, due to increasing resistance and lack of development of new agents, the possibility of a return to the pre-antimicrobial era may become a reality.
So how were infections treated before antimicrobials were developed in the early 20th century?
Blood, leeches and knives
Bloodletting was used as a medical therapy for over 3,000 years. It originated in Egypt in 1000 B.C. and was used until the middle of the 20th century.
Medical texts from antiquity all the way up until 1940s recommend bloodletting for a wide variety of conditions, but particularly for infections. As late as 1942, William Osler’s 14th edition of Principles and Practice of Medicine, historically the preeminent textbook of internal medicine, included bloodletting as a treatment for pneumonia.
Bloodletting is based on an ancient medical theory that the four bodily fluids, or “humors” (blood, phlegm, black bile and yellow bile), must remain in balance to preserve health. Infections were thought to be caused by an excess of blood, so blood was removed from the afflicted patient.
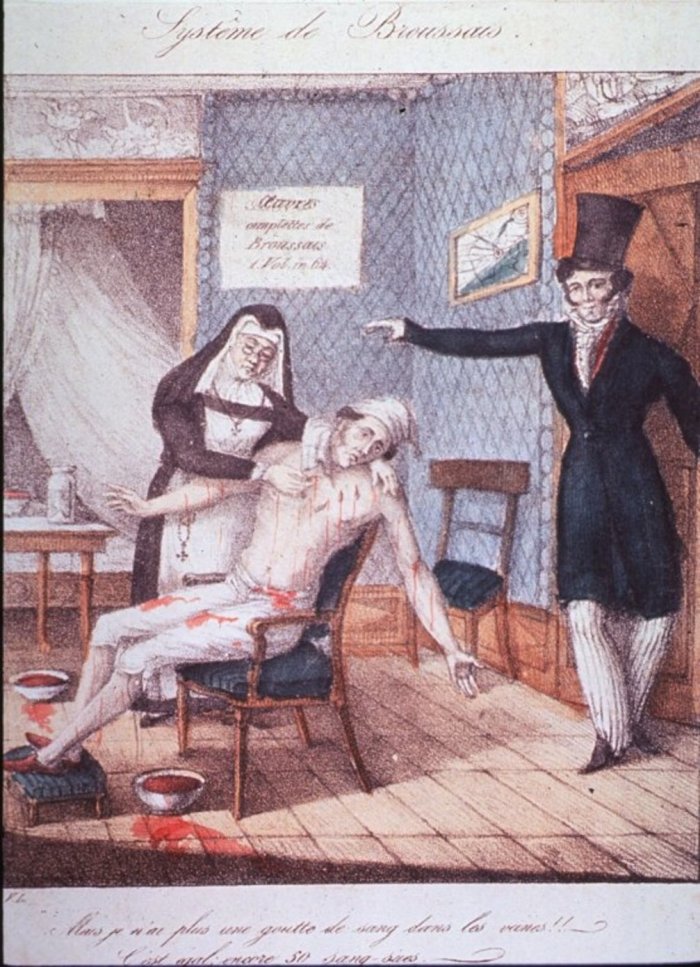
One method was to make an incision in a vein or artery, but it was not the only one. Cupping was another common method, in which heated glass cups were placed on the skin, creating a vacuum, breaking small blood vessels and resulting in large areas of bleeding under the skin. Most infamously, leeches were also used as a variant of bloodletting.
Interestingly, though bloodletting was recommended by physicians, the practice was actually performed by barbers, or “barber-surgeons.” The red and white striped pole of the barbershop originated as “advertising” their bloodletting services, the red symbolizing blood and the white symbolizing bandages.
There may actually have been some benefit to the practice – at least for certain kinds of bacteria in the early stages of infection. Many bacteria require iron to replicate, and iron is carried on heme, a component of the red blood cell. In theory, fewer red blood cells resulted in less available iron to sustain the bacterial infection.
Some mercury for your syphilis?
Naturally occurring chemical elements and chemical compounds have historically have been used as therapies for a variety of infections, particularly for wound infections and syphilis.
Topical iodine, bromine and mercury-containing compounds were used to treat infected wounds and gangrene during the American Civil War. Bromine was used most frequently, but was very painful when applied topically or injected into a wound, and could cause tissue damage itself. These treatments inhibited bacterial cell replication, but they could also harm normal human cells.
Mercury compounds were used to treat syphilis from about 1363 to 1910. The compounds could be applied to skin, taken orally or injected. But the side effects could include extensive damage to skin and mucous membranes, kidney and brain damage, and even death. Arsphenamine, an arsenic derivative, was also used in the first half of the 20th century. Though it was effective, side effects included optic neuritis, seizures, fever, kidney injury and rash.
Thankfully, in 1943, penicillin supplanted these treatments and remains the first-line therapy for all stages of syphilis.
Looking in the garden
Over the centuries, a variety of herbal remedies evolved for the treatment of infections, but very few have been evaluated by controlled clinical trials.
One of the more famous herbally derived therapies is quinine, which was used to treat malaria. It was originally isolated from the bark of the cinchona tree, which is native to South America. Today we use a synthetic form of quinine to treat the disease. Before that, cinchona bark was dried, ground into powder, and mixed with water for people to drink. The use of cinchona bark to treat fevers was described by Jesuit missionaries in the 1600s, though it was likely used in native populations much earlier.
Artemisinin, which was synthesized from the Artemisia annua (sweet wormwood) plant is another effective malaria treatment. A Chinese scientist, Dr. Tu Youyou, and her team analyzed ancient Chinese medical texts and folk remedies, identifying extracts from Artemisia annuaas effectively inhibiting the replication of the malaria parasite in animals. Tu Youyou was coawarded the 2015 Nobel Prize in Physiology or Medicine for the discovery of artemisinin.
You probably have botantically derived therapy against wound infection in your kitchen cupboard. The use of honey in wound healing dates back to the Sumerians in 2000 B.C.. The high sugar content can dehydrate bacterial cells, while acidity can inhibit growth and division of many bacteria. Honey also has an enzyme, glucose oxidase, that reduces oxygen to hydrogen peroxide, which kills bacteria.
The most potent naturally occurring honey is thought to be Manuka honey. It is derived from the flower of the tea tree bush, which has additional antibacterial properties.
Like other botanically derived therapies, honey has inspired the creation of pharmaceuticals. MEDIHONEY®, a medical grade product developed by Derma Sciences, is used to promote healing in burns as well as other types of wounds.
Combating antimicrobial resistance
While some of these ancient therapies proved effective enough that they are still used in some form today, on the whole they just aren’t as good modern antimicrobials at treating infections. Sadly, thanks to overuse and misuse, antibiotics are becoming less effective.
Each year in the United States, at least two million people become infected with bacteria that are resistant to antibiotics, and at least 23,000 people die each year as a direct result of these infections.
While resistant bacteria are most commonly reported, resistance also can arise in other microorganisms, including fungi, viruses and parasites. Increasing resistance has raised the possibility that certain infections may eventually be untreatable with the antimicrobials we currently have.
The race is on to find new treatments for these infections, and researchers are exploring new therapies and new sources for antibiotics.
Besides using antibiotics as directed and only when necessary, you can avoid infections in the first place with appropriate immunization, safe food-handling practices and washing your hands.
Tracking resistant infections so we can learn more about them and their risk factors, as well as limiting the use of antibiotics in humans and animals, could also help curb the risk of resistant bacteria.
MessageToEagle.com
via Conversation






